Plantar Fasciitis
What is Plantar Fasciitis?
Plantar Fasciitis is the common name for Plantar Fasciosis.
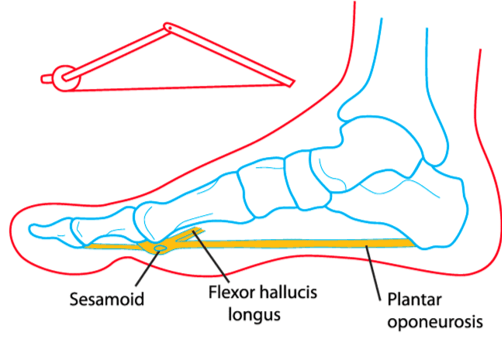
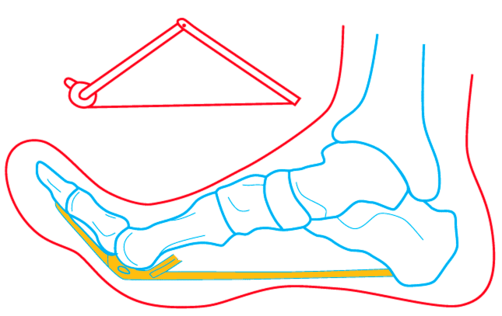
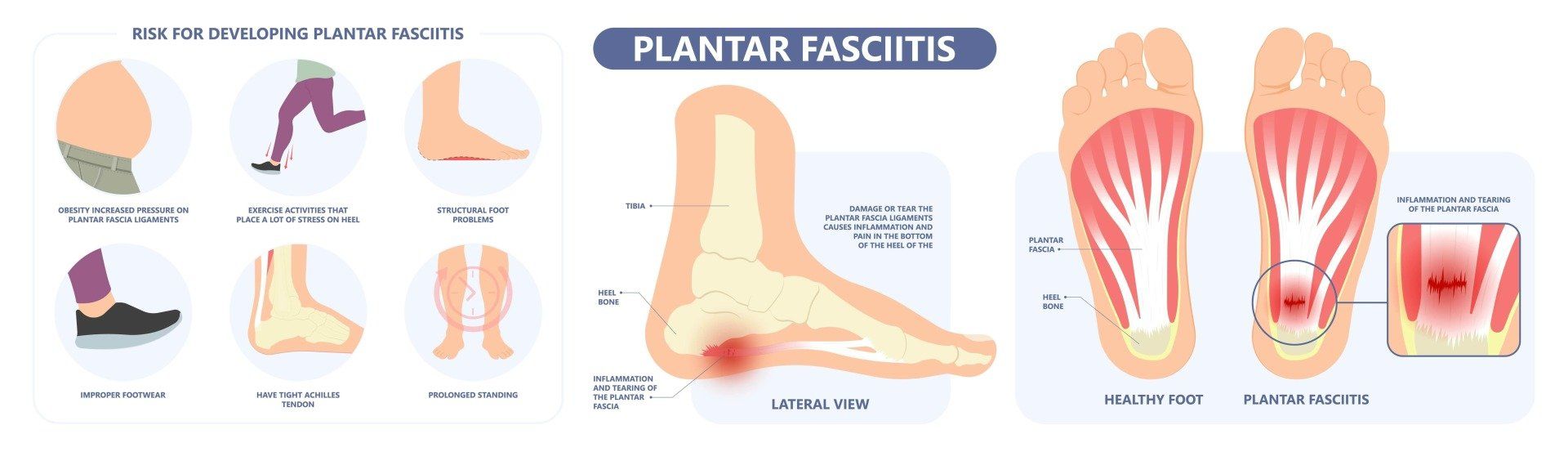
Conditions that end in "-itis" denote inflammation. It is more correctly called Plantar Fasciosis because while there are inflammatory chemicals that cause pain, no actual inflammatory cells are found within the plantar fascia. The plantar fascia a strong, elastic band of collagen tissue that lies at the bottom of the foot. It runs from the heel bone to the toe and forms the arch of your foot.
Plantar Fasciitis is one of the most common causes of heel pain. It is most often seen in middle-aged men and women, but may also occur in those who are constantly on their feet such as soldiers, hairdressers, mechanics and construction workers.
Plantar heel pain, pain under the heel, can be caused by many different sources.
In most cases it is the medial band of the plantar fascia that is overloaded as it inserts into the medial part of the heel bone.
However, there are other important problems that can occur including a stress fracture or bone bruising of the heel bone, entrapment of the inferior branch of the lateral plantar nerve which tends to create more burning pain and even bruising and inflammation of the fat pad underneath the heel. See the video above for further anatomical detail.
This area of the body takes an enormous amount of both tensile and compressive load, so it doesn’t take much to develop problems here.
Plantar fasciitis is more correctly called plantar fasciosis or fasciopathy because it is not a classically inflammatory problem, even if some inflammatory chemicals are present.
It is a very common presentation to Sports physicians because surgery is an absolute last resort and conservative management, and time are usually effective.
The duration of symptoms can be anywhere from months to years, but most cases resolve with treatment.
What are the Causes or Risk Factors of Plantar Fasciitis?
Mechanical Factors
The plantar fascia functions as a biological spring that stores and releases energy for propulsion, and supports the arch of your foot. Excessive pressure over the fascia may strain and tear the tissue causing heel pain. Repeated overstretching or overuse causes irritation or inflammation of the fascia.
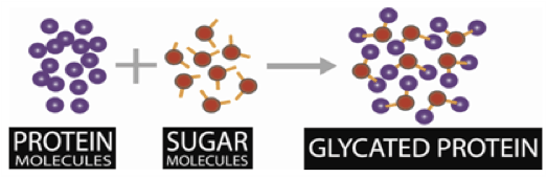
Metabolic Factors
While not fully understood, metabolic factors seem to be important too, since diabetics have 5x the risk of plantar fasciitis and the thickness of the plantar fascia has been shown to correlate with blood sugar control.
Other Factors
Other risk factors may include obesity, foot arch problems such as flat feet or high arches, activities such as long-distance running, ballet and dance aerobics, occupations that necessitate walking or standing on hard surfaces for a long period, and wearing shoes with poor arch support or thin-soled shoes.
Symptoms of Plantar Fasciitis
The most common symptom is sharp pain on the bottom of the foot near the heel. You experience pain when you take your first steps on awakening and it slowly decreases but may return after standing for a long period.
Diagnosis of Plantar Fasciitis
Patients who suspect they have sustained Plantar Fasciitis should seek a medical consultation. While it is the most common cause for pain under the heel, there are other causes that require attention to detail to diagnose. The diagnosis for a Plantar Fasciitis can often include:
Physical Examination
The affected part of the heel is evaluated to determine the presence of swelling, a limited range of motion anywhere in the lower limb, abnormal walking biomechanics, and focal tenderness on the inside of the heel bone where the plantar fascia inserts. Pain with squeezing the heel bone can indicate a Calcaneal stress fracture), while irritation of the local nerves can indicate a Baxter's neuropathy. These are commonly missed.
Obtain a Full Medical History
You will be asked about your symptoms, medical history, any sports participation and activities that aggravate your condition.
Prior injury can elevate an athlete’s risk of sustaining an injury to the foot or ankle. Metabolic problems also increase the risk of plantar fasciitis. With this in mind, Dr Samra will take a thorough medical history in order to determine if a former condition has contributed and needs to be addressed.
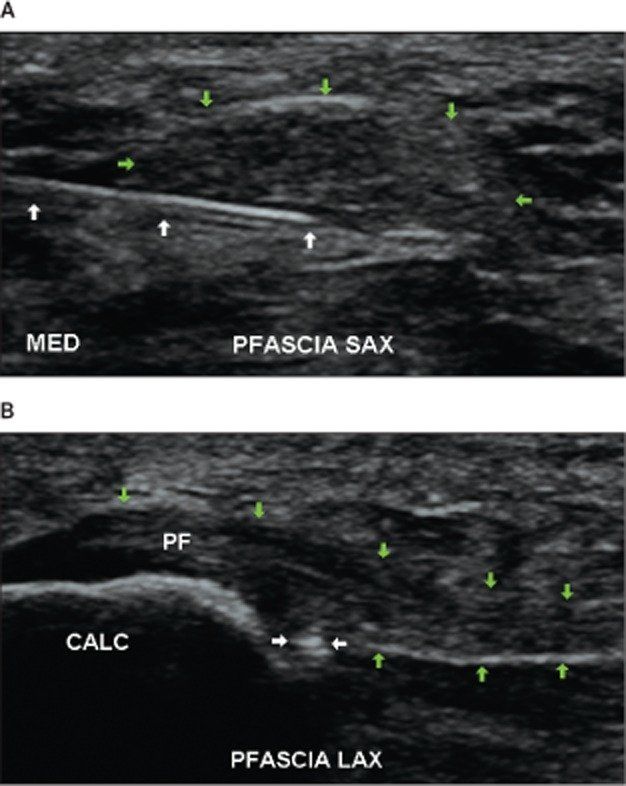
Medical Imaging
Dr Samra will perform an ultrasound to look at your plantar fascia and surrounding tissues, as an extension of the physical examination of the foot or ankle. Following this, medical imaging such as an X-ray or Magnetic Resonance Imaging (MRI) can help to form a final diagnosis.
A comprehensive evaluation of the patient’s foot or ankle allows Dr Samra to eliminate various possibilities, arrive at a diagnosis, and recommend a treatment plan.
Recommended Treatments for Plantar Fasciitis
Following a medical evaluation, your doctor will be able to recommend a course of treatment. Here is a helpful checklist of treatments for plantar fasciitis, to help you determine whether you need to escalate to seeing a Sport and Exercise Physician:
Evidence-Based Exercises
Are you providing stimulus for your plantar fascia to become stronger?
- Stretches to the plantar fascia, calves and hamstrings and foot exercises
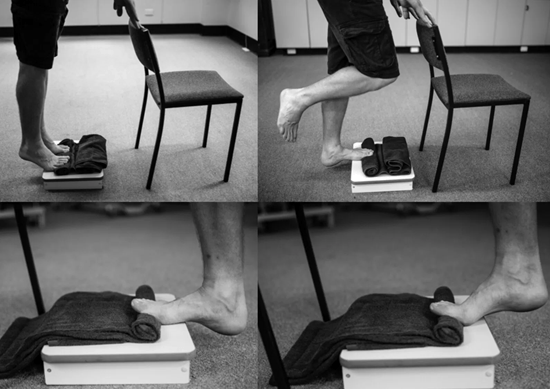
- Calf raises with toe bent up (Windlass raises- see below) (3)
- Adherence to exercises (second daily) for AT LEAST 8 weeks
Danish Physiotherapist and researcher, Michael Rathleff, performed an excellent study that demonstrated the effectiveness of exercises for plantar fasciitis. A Physiotherapist can prescribe, supervise and progress these exercises.
Activity Modification
Are you optimising the load stimulus for the tissue to adapt appropriately?
- Step counter (e.g. fitbit)- keeping steps under 5,000 (or whatever works to control pain) in the early stages
- Temporarily STOP running or impact activities
- Using a spin bike low resistance to supplement exercise
- Any activity you know that flares pain
- A walking boot is rarely required and can lead to calf and ankle weakness
Lifestyle
Are you optimising the internal environment for healing?
- Smoking cessation
- Dietary change and weight loss if relevant
Footwear
Have you found any footwear that is comfortable?
- Closed cushioned shoes at most times (avoid bare feet) including out of bed
- Podiatrist review for advice, tape and footwear review
- Soft inserts- silicone heel cups or arch supports (1)
- Night splints: Use night splints such as a "Strassberg Sock" to stretch the plantar fascia improve pain. (2)
Physical Modalities
Have you found any benefit from physical modalities to help you do exercises?
- Massage: Calf through to the big toe can improve pain (4–6)
- Ice: ice pack or ice in a bottle roller for pain. There is no inflammation so this is not strongly advised.
- Acupuncture: This is painful around the heel, and can irritate the local nerves. I would recommend avoidance.
- Laser (10,11): Focused laser has been used to heat the underlying tissue.
- Extracorporeal shockwave treatment: This procedure, also known as ESWT, involves sending sound-wave impulses into the tissue to desensitise the local nerve-endings, and possibly to help induce adaptive tissue changes. (12–15)
Injectable Treatments
Failing the above, have you tried any injectable treatments for pain?
- Cortisone injection
- Platelet-rich plasma therapy: This practice, also known as PRP, involves injecting the site of the injury with the patient's own platelet-rich plasma in an effort to accelerate healing.
- Prolotherapy Injections
Surgery
Occasionally, surgery to release the tight plantar fascia may be needed. Plantar Fascia Surgery (Endoscopic) also known as Endoscopic Plantar Fasciotomy (EPF), is a procedure used to remove a small portion of Plantar Fascia when the fascia becomes tightened or is contracted to cause inflammation and pain.
Minimally invasive forms of this procedure (Percutaneous Tenotomy) are now being performed to reduce surgical risk, but these are not yet available in Australia.
This surgery releases the tension and allows relief from inflammation. While there are risks of nerve and vascular injury, the outcome of this procedure is generally good with an overall 90% success rate.
Reference List
- Craig ME, Duffin AC, Gallego PH, Lam A, Cusumano J, Hing S, et al. Plantar fascia thickness, a measure of tissue glycation, predicts the development of complications in adolescents with type 1 diabetes. Diabetes Care. 2008 Jun;31(6):1201–6.
- Gautieri A, Passini FS, Silván U, Guizar-Sicairos M, Carimati G, Volpi P, et al. Advanced glycation end-products: Mechanics of aged collagen from molecule to tissue. Matrix Biol. 2017 May;59:95–108.
- Buchbinder R. Clinical practice. Plantar fasciitis. N Engl J Med. 2004 May 20;350(21):2159–66.
- De Garceau D, Dean D, Requejo SM, Thordarson DB. The association between diagnosis of plantar fasciitis and Windlass test results. Foot Ankle Int. 2003 Mar;24(3):251–5.
- Riddle DL, Pulisic M, Pidcoe P, Johnson RE. Risk factors for Plantar fasciitis: a matched case-control study. J Bone Joint Surg Am. 2003 May;85-A(5):872–7.
- McPoil TG, Martin RL, Cornwall MW, Wukich DK, Irrgang JJ, Godges JJ. Heel pain--plantar fasciitis: clinical practice guildelines linked to the international classification of function, disability, and health from the orthopaedic section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2008 Apr;38(4):A1–18.
- Rathleff MS, Mølgaard CM, Fredberg U, Kaalund S, Andersen KB, Jensen TT, et al. High-load strength training improves outcome in patients with plantar fasciitis: A randomized controlled trial with 12-month follow-up. Scand J Med Sci Sports. 2015 Jun;25(3):e292-300.
- Chew KTL, Leong D, Lin CY, Lim KK, Tan B. Comparison of autologous conditioned plasma injection, extracorporeal shockwave therapy, and conventional treatment for plantar fasciitis: a randomized trial. PM R. 2013 Dec;5(12):1035–43.
- Jain K, Murphy PN, Clough TM. Platelet rich plasma versus corticosteroid injection for plantar fasciitis: A comparative study. Foot Edinb Scotl. 2015 Dec;25(4):235–7.
- McMillan AM, Landorf KB, Gilheany MF, Bird AR, Morrow AD, Menz HB. Ultrasound guided corticosteroid injection for plantar fasciitis: randomised controlled trial. BMJ. 2012 May 22;344:e3260.
- Porter MD, Shadbolt B. Intralesional corticosteroid injection versus extracorporeal shock wave therapy for plantar fasciopathy. Clin J Sport Med Off J Can Acad Sport Med. 2005 May;15(3):119–24.
- Roos E, Engström M, Söderberg B. Foot orthoses for the treatment of plantar fasciitis. Foot Ankle Int. 2006 Aug;27(8):606–11.
- Mizel MS, Marymont JV, Trepman E. Treatment of plantar fasciitis with a night splint and shoe modification consisting of a steel shank and anterior rocker bottom. Foot Ankle Int. 1996 Dec;17(12):732–5.
- DiGiovanni BF, Nawoczenski DA, Lintal ME, Moore EA, Murray JC, Wilding GE, et al. Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain. A prospective, randomized study. J Bone Joint Surg Am. 2003 Jul;85-A(7):1270–7.
- Kamonseki DH, Gonçalves GA, Yi LC, Júnior IL. Effect of stretching with and without muscle strengthening exercises for the foot and hip in patients with plantar fasciitis: A randomized controlled single-blind clinical trial. Man Ther. 2015 Oct 30;
- Boules M, Batayyah E, Froylich D, Zelisko A, O’Rourke C, Brethauer S, et al. Effect of Surgical Weight Loss on Plantar Fasciitis and Health-Care Use. J Am Podiatr Med Assoc. 2018 Nov;108(6):442–8.
- Donley BG, Moore T, Sferra J, Gozdanovic J, Smith R. The efficacy of oral nonsteroidal anti-inflammatory medication (NSAID) in the treatment of plantar fasciitis: a randomized, prospective, placebo-controlled study. Foot Ankle Int. 2007 Jan;28(1):20–3.
- Aqil A, Siddiqui MRS, Solan M, Redfern DJ, Gulati V, Cobb JP. Extracorporeal Shock Wave Therapy Is Effective In Treating Chronic Plantar Fasciitis: A Meta-analysis of RCTs. Clin Orthop. 2013 Nov;471(11):3645–52.
- Ibrahim MI, Donatelli RA, Schmitz C, Hellman MA, Buxbaum F. Chronic Plantar Fasciitis Treated with Two Sessions of Radial Extracorporeal Shock Wave Therapy. Foot Ankle Int. 2010 May;31(5):391–7.
- Franceschi F, Papalia R, Franceschetti E, Paciotti M, Maffulli N, Denaro V. Platelet-rich plasma injections for chronic plantar fasciopathy: a systematic review. Br Med Bull. 2014 Dec;112(1):83–95.