Metabolic Health Clinic
Medical Causes of Weight Gain are Real
Weight gain and obesity are not simply diseases of over-nourishment. Whilst there is certainly an "obesogenic environment" that we currently live in, there are contributions from medical conditions. Often these conditions remain undiagnosed for years, while patients undertake apparently futile attempts at diet and exercise without results or knowledge of any meaningful metabolic change.
In mainstream media there is often talk of endocrine disorders such as hypothyroidism, cushings disease and even pituitary tumours as causes of weight gain. These are relatively rare.
INSULIN RESISTANCE
The most common cause of weight gain and inhibition of weight loss
This is not taught well, if at all, in most medical courses. If you are interested in understanding this problem and what to do about it, please see the video below.
Is Visceral Fat associated with Injury and Pain?
Absolutely yes. When we think of musculoskeletal pain, we often think about tissue injury.
However, it’s important to realise that many of the chronic and recalcitrant problems we see in musculoskeletal medicine are contributed to strongly by metabolic health. And it goes far beyond simply putting more stress on your joints...
We see a huge range of patients in our clinic from “metabolic perfection with” highly insulin sensitive and fuel-efficient athletes to “metabolically sick” diabetic patients with severely elevated blood glucose levels damaging their small and large blood vessels, and everything between.
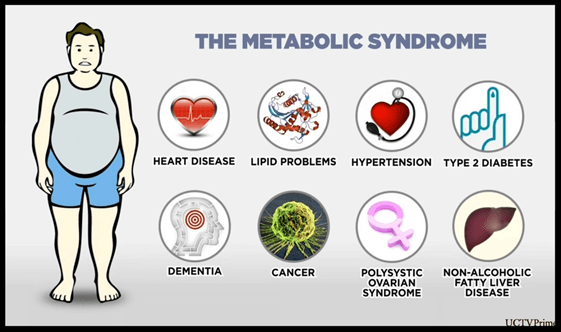
When we look at patients at the sickest end of the metabolic spectrum, we see a rampant increase in many of the chronic disorders including:
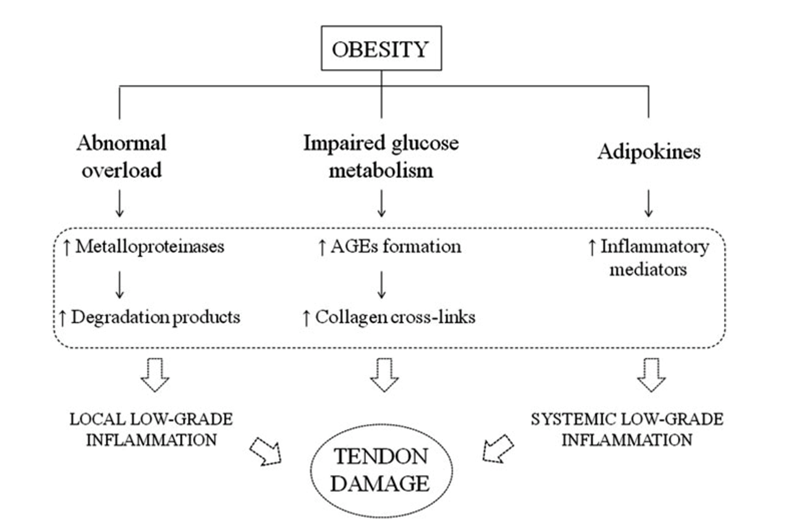
Tendon pain- such as achilles pain, increased by 350%. Any and all other tendon problems like tennis elbow, jumpers knee, rotator cuff wear and trigger finger fall under this category.1–3
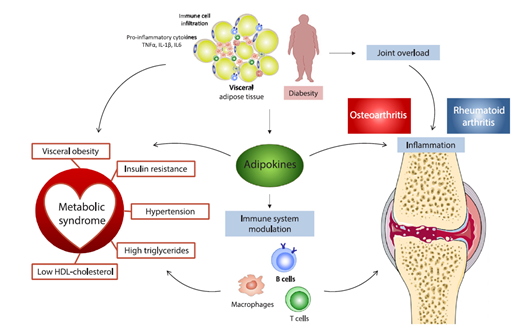
Osteaoarthritis- increased by 150%. 4 And it’s not just driven by BODY WEIGHT and extra joint loads. We see that high insulin levels independently associated with osteoarthritis.5 Also, Patients with hand arthritis have as much as a 40-50% improvement in their pain when they lose 5-10% body weight.6
Frozen shoulder or adhesive capsulitis- 500% increase 7,8
Plantar fasciitis (more correctly termed plantar fasciosis)- 165% increase
9
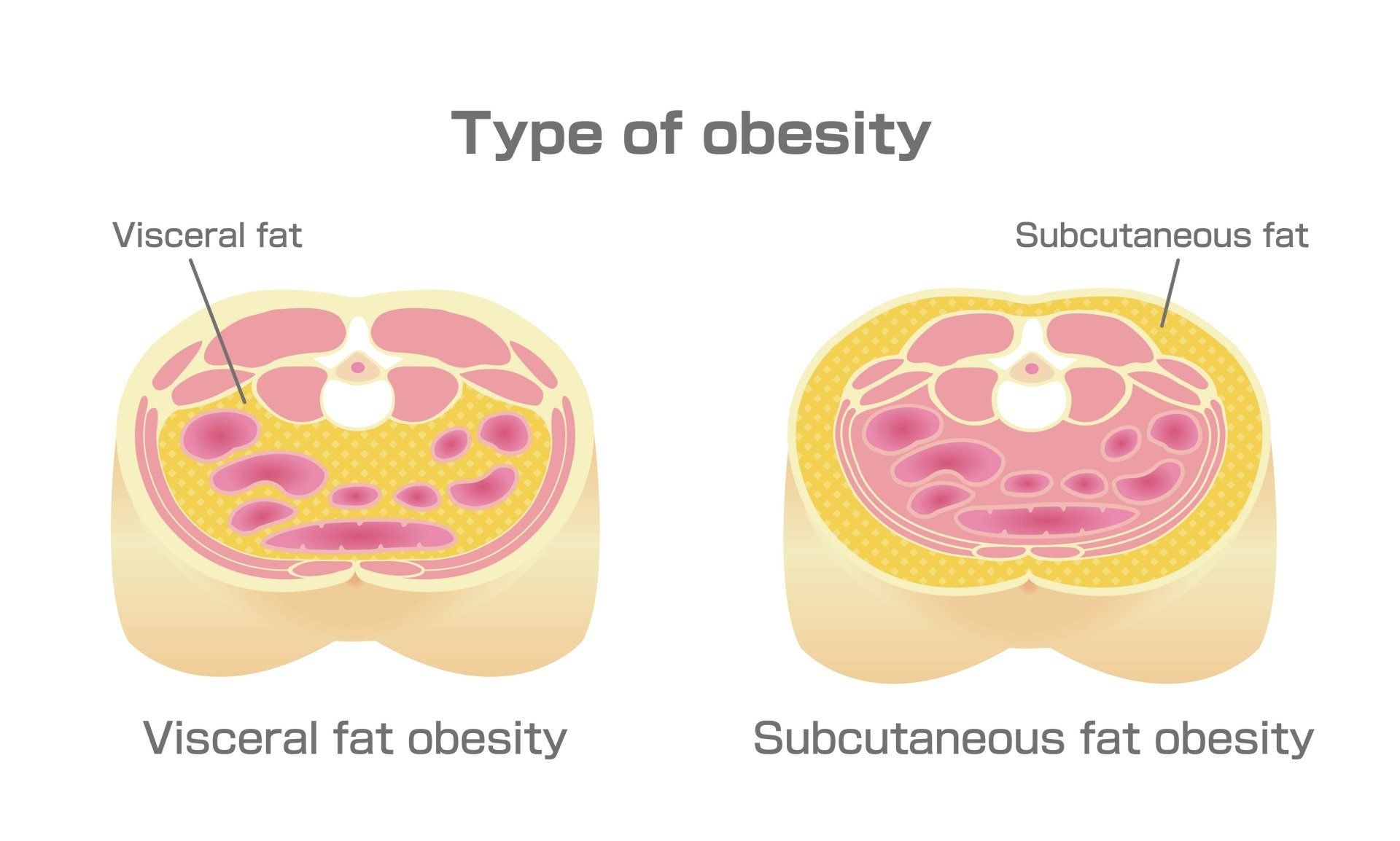
We know that chronically high insulin levels leads to fat accumulation around the abdominal organs, and this so called VISCERAL fat is strongly pro-inflammatory as it releases chemicals called adipokines. 12–15 At any moment, an ageing human has some wear and tear all over their body, but this just means that those things are much more likely to cause inflammation and the pain that goes with that.
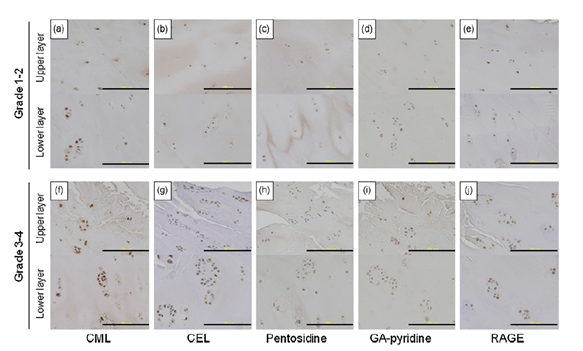
We also know that spikes of glucose and chronically elevated glucose levels lead to glucose binding to our proteins and damaging them. This process is called glycation and produces advanced glycation end products, which is pretty much the same process of browning or caramelization of your own tissues like your tendons, joints, lens in the eye and more. Here you can see this process shown by the browning of rib cartilage played out through the lifespan. The same thing has been shown with increasing grades of osteoarthritis affecting cartilage in our joints. 16,17
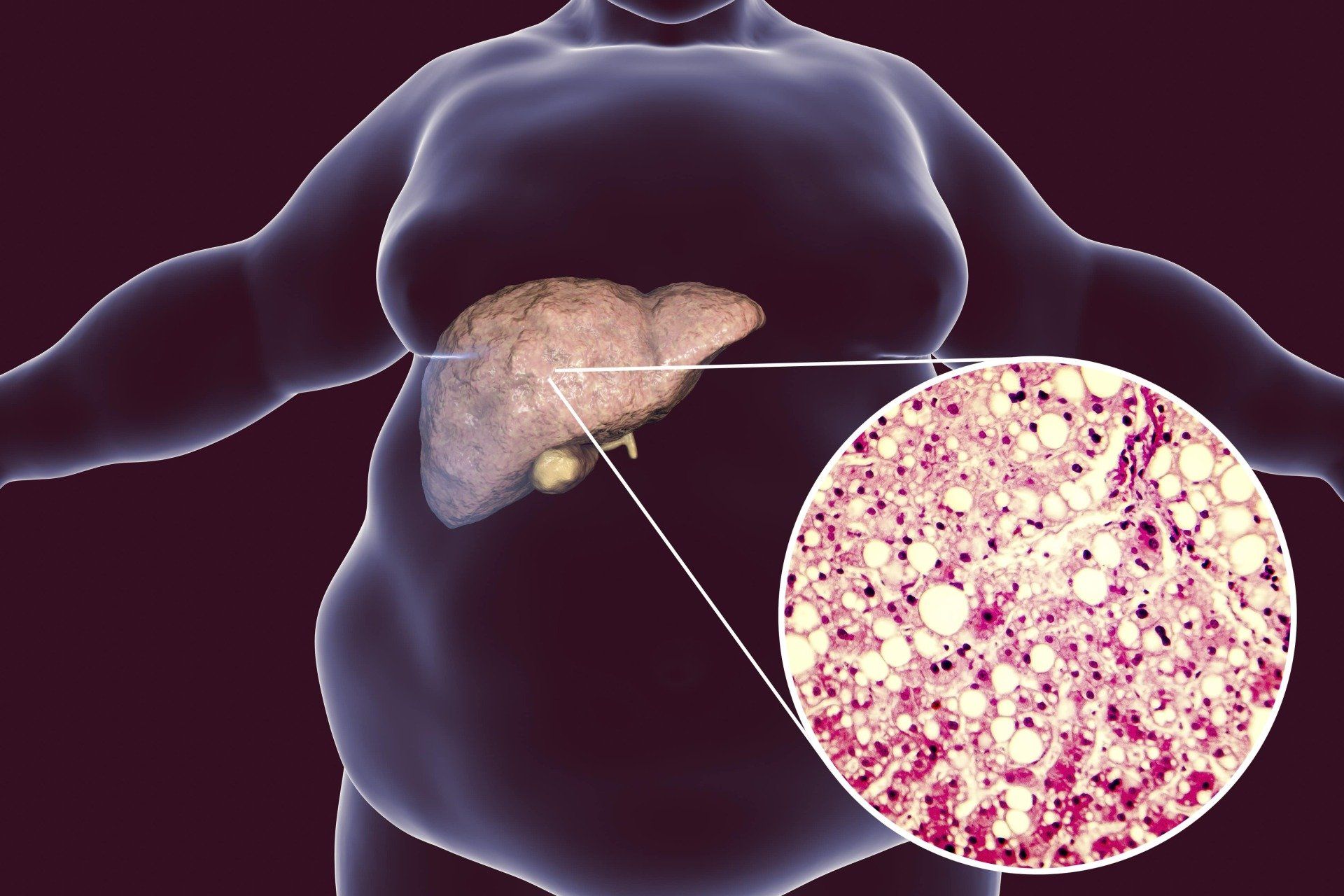
Finally, the accumulation of fat in the liver known as non-alcoholic fatty liver disease or NAFLD can lead the liver to erratically produce enzymes called MMPs that degrade tissue matrix such as in cartilage and tendons. 18–20
While it is important to address local sources for pain and optimize the loading conditions for recovery, undertaking lifestyle changes is also of great value to many patients suffering these conditions as a manifestation of poor metabolic health, before more significant health issues arise.
There are different ways to achieve a low insulin lifestyle, and if you’ve struggled with multiple musculoskeletal issues, please take a look at my educational series outlining the theory and application of this intervention below.
What can I do about my Metabolic Health?
The Low Insulin Lifestyle is a term I coined in trying to address two important facts:
Diets don't work long-term, lifestyles do.
The Hormonal Model of weight gain explains human behaviour and physiology much better than the Calorie Model
Understanding Insulin Resistance is at the heart of managing the metabolic syndrome and obesity.
The Video Series below outlines the approach and practical principles of achieving a low insulin lifestyle and how to be scientific about this approach to ensure long-term success.
How Does Weight Gain Affect You?
Obesity substantially contributes to
- Preventable, non-communicable diseases,
- Musculoskeletal Pain
- Shortened life-expectancy and
- Impaired quality of life.
- Systemic Inflammation (making existing injuries HURT more)
Doctors and Scientists hypothesise that obesity may be a protective mechanism against the development of hyperglycemia and diabetes.
It exists along the spectrum of symptoms of persistently high insulin levels, or the "metabolic syndrome"
Poor metabolic health is associated with:
- Type 2 Diabetes
- Musculoskeletal disorders (joint pain, bursitis, ligament and tendon damage as above)
- Heart disease, Hypertension and Stroke
- Depression, Anxiety and Cognitive Decline
What are the Causes of Obesity?
Weight gain and long-term obesity can be caused by a number of factors:
- Genetic susceptibility
- Development of insulin resistance, starting at the level of muscle tissue with deposition of diacylglycerol
- Habitual high sugar intake leading to de novo lipogenesis
- Habitual high carbohydrate intake maintaining de novo lipogenesis
- High alcohol intake (also leading to fatty liver)
- Hormonal abnormalities (such as PCOS, Hyperinsulinemia Syndrome, Prada-Wili syndrome, Hypothyroidism, Cushing's syndrome)
- High caloric intake secondary to the above factors
- Physical Inactivity and Sarcopenia (loss of muscle mass)
Affiliations
Dr Samra has no commercial conflicts of interest and does not invest in or advise any companies.
The following affiliations are for the benefit of patients' further education and information.
Reference List
- Baskerville R, McCartney DE, McCartney SM, Dawes H, Tan GD. Tendinopathy in type 2 diabetes: a condition between specialties? Br J Gen Pract. 2018 Dec;68(677):593–4.
- Lui PPY. Tendinopathy in diabetes mellitus patients-Epidemiology, pathogenesis, and management. Scand J Med Sci Sports. 2017 Aug;27(8):776–87.
- Ranger TA, Wong AMY, Cook JL, Gaida JE. Is there an association between tendinopathy and diabetes mellitus? A systematic review with meta-analysis. Br J Sports Med. 2016 Aug;50(16):982–9.
- Louati K, Vidal C, Berenbaum F, Sellam J. Association between diabetes mellitus and osteoarthritis: systematic literature review and meta-analysis. RMD Open [Internet]. 2015 Jun 2 [cited 2020 May 15];1(1). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4613158/
- Silveri F, Brecciaroli D, Argentati F, Cervini C. Serum levels of insulin in overweight patients with osteoarthritis of the knee. J Rheumatol. 1994 Oct;21(10):1899–902.
- Yusuf E, Nelissen RG, Ioan-Facsinay A, Stojanovic-Susulic V, DeGroot J, van Osch G, et al. Association between weight or body mass index and hand osteoarthritis: a systematic review. Ann Rheum Dis. 2010 Apr;69(4):761–5.
- Zreik NH, Malik RA, Charalambous CP. Adhesive capsulitis of the shoulder and diabetes: a meta-analysis of prevalence. Muscles Ligaments Tendons J. 2016 May 19;6(1):26–34.
- Austin DC, Gans I, Park MJ, Carey JL, Kelly JD. The association of metabolic syndrome markers with adhesive capsulitis. J Shoulder Elbow Surg. 2014 Jul;23(7):1043–51.
- Priesand SJ, Schmidt BM, Ang L, Wrobel JS, Munson M, Ye W, et al. Plantar fasciitis in patients with type 1 and type 2 diabetes: A contemporary cohort study. J Diabetes Complications. 2019 Oct;33(10):107399.
- Cameron AJ, Magliano DJ, Zimmet PZ, Welborn T, Shaw JE. The Metabolic Syndrome in Australia: Prevalence using four definitions. Diabetes Res Clin Pract. 2007 Sep;77(3):471–8.
- Ervin RB. Prevalence of Metabolic Syndrome Among Adults 20 Years of Age and Over, by Sex, Age, Race and Ethnicity, and Body Mass Index: United States,. 2009;(13):8.
- de Boer TN, van Spil WE, Huisman AM, Polak AA, Bijlsma JWJ, Lafeber FPJG, et al. Serum adipokines in osteoarthritis; comparison with controls and relationship with local parameters of synovial inflammation and cartilage damage. Osteoarthritis Cartilage. 2012 Aug;20(8):846–53.
- Francisco V, Ruiz-Fernández C, Pino J, Mera A, González-Gay MA, Gómez R, et al. Adipokines: Linking metabolic syndrome, the immune system, and arthritic diseases. Biochem Pharmacol. 2019 Jul;165:196–206.
- Zheng S, Xu J, Xu S, Zhang M, Huang S, He F, et al. Association between circulating adipokines, radiographic changes, and knee cartilage volume in patients with knee osteoarthritis. Scand J Rheumatol. 2016;45(3):224–9.
- Jung UJ, Choi M-S. Obesity and Its Metabolic Complications: The Role of Adipokines and the Relationship between Obesity, Inflammation, Insulin Resistance, Dyslipidemia and Nonalcoholic Fatty Liver Disease. Int J Mol Sci. 2014 Apr 11;15(4):6184–223.
- Hirose J, Yamabe S, Takada K, Okamoto N, Nagai R, Mizuta H. Immunohistochemical distribution of advanced glycation end products (AGEs) in human osteoarthritic cartilage. Acta Histochem. 2011 Oct;113(6):613–8.
- Saudek DM, Kay J. Advanced glycation endproducts and osteoarthritis. Curr Rheumatol Rep. 2003 Feb;5(1):33–40.
- Murata K, Uchida K, Takano S, Shoji S, Iwase D, Inoue G, et al. Osteoarthritis patients with high haemoglobin A1c have increased Toll-like receptor 4 and matrix metalloprotease-13 expression in the synovium. Diabetes Metab Syndr Obes Targets Ther. 2019 Jul 16;12:1151–9.
- Kostopoulou F, Malizos KN, Papathanasiou I, Tsezou A. MicroRNA-33a regulates cholesterol synthesis and cholesterol efflux-related genes in osteoarthritic chondrocytes. Arthritis Res Ther. 2015;17(1):42.
- Loeser RF, Beavers DP, Bay-Jensen AC, Karsdal MA, Nicklas BJ, Guermazi A, et al. Effects of Dietary Weight Loss with and without Exercise on Interstitial Matrix Turnover and Tissue Inflammation Biomarkers in Adults with Knee Osteoarthritis: The Intensive Diet and Exercise for Arthritis Trial (IDEA). Osteoarthritis Cartilage. 2017 Nov;25(11):1822–8.