Integrating Tech for Improved Patient Care
Why we embrace technology at PSM

Introduction
In the rapidly evolving field of healthcare, embracing technology is no longer an option; it's a necessity. As a Sport and Exercise Physician, I have seen firsthand the transformative impact that integrating the right tools can have on patient outcomes. At Progressive Sports Medicine, our mission is clear: Empower Health through Science and Education. In this blog, I want to share insights into how we can leverage technology and collaboration to build better patient outcomes, cutting out administrative inefficiencies and maximizing the value of our patient interactions
The Last Five Years: Lessons in Adaptation
The journey to establishing my own clinic was catalyzed by a particularly harsh Google review that highlighted system deficiencies. This experience ingrained a crucial lesson: "We rise to the level of our goals, but we fall to the level of our systems." Taking full ownership of the patient experience has empowered me to explore every facet of practice management. This journey of embracing vulnerability and seeking constant improvement has been central to the growth of my practice
Embracing Vulnerability in Healthcare
Being fearless in healthcare isn't about avoiding technology; it's about using it to objectively assess our outcomes. It's about listening to our patients, understanding their needs, and striving for better outcomes. For instance, the high cancellation rates among metabolic patients often stem from their fear of perceived failure. By focusing not just on treatment but on patient education, we can shift them from passive participants to engaged partners in their healthcare journey

Integrating Workflow Technology
Why should we bother with workflow technology? The answer is simple: it makes everything smoother. At Progressive Sports Medicine, we use tools like Google Workspace and 3CX to streamline communication and prioritize tasks. These technologies automate repetitive tasks, answer frequently asked questions, and allow us to focus on solving real problems. The integration of whisper AI transcription software, for example, has enabled us to provide real-time feedback and training to our reception staff, enhancing the overall patient experience
The Power of Patient Portals
A carefully thought-out patient portal is a game-changer in empowering patients. It allows patients to stay informed about their condition and track their progress even before stepping into the clinic. This ongoing engagement not only keeps patients motivated but also ensures that both patients and practitioners get the maximum value from their time together

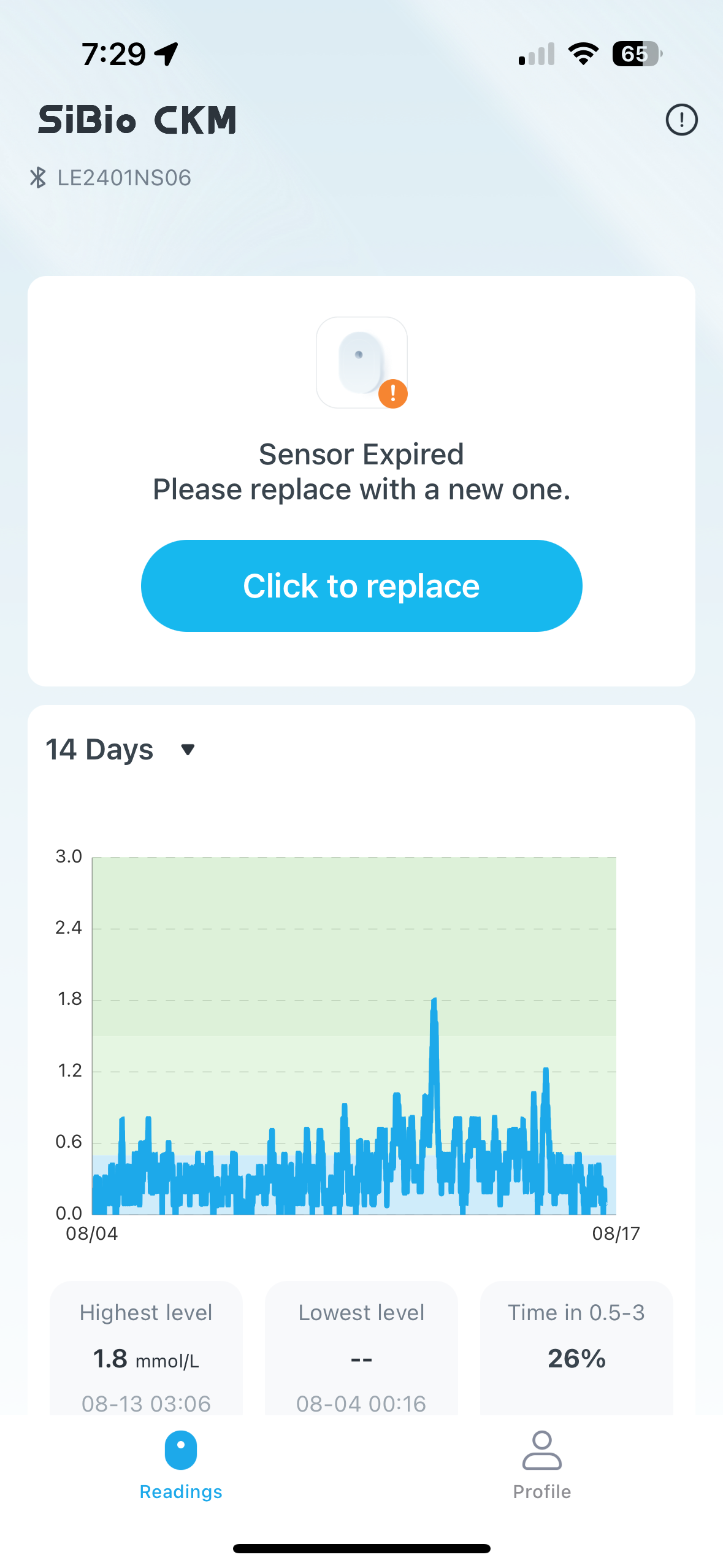
Empowering Patients with Biofeedback Technology
Continuous Glucose Monitors (CGMs) and Continuous Ketone Monitors are powerful tools that provide real-time feedback, helping patients manage their health more effectively. By monitoring glucose levels or ketosis in real-time, patients can make informed decisions about their diet and exercise, leading to better health outcomes. For example, studies have shown that CGMs are effective in improving glucose control in diabetics, reducing the long-term harms of poor glycemic control. Continuous Ketone Monitors are newer on the market and provide some very important insights into metabolic flexibility when harnessed correctly.
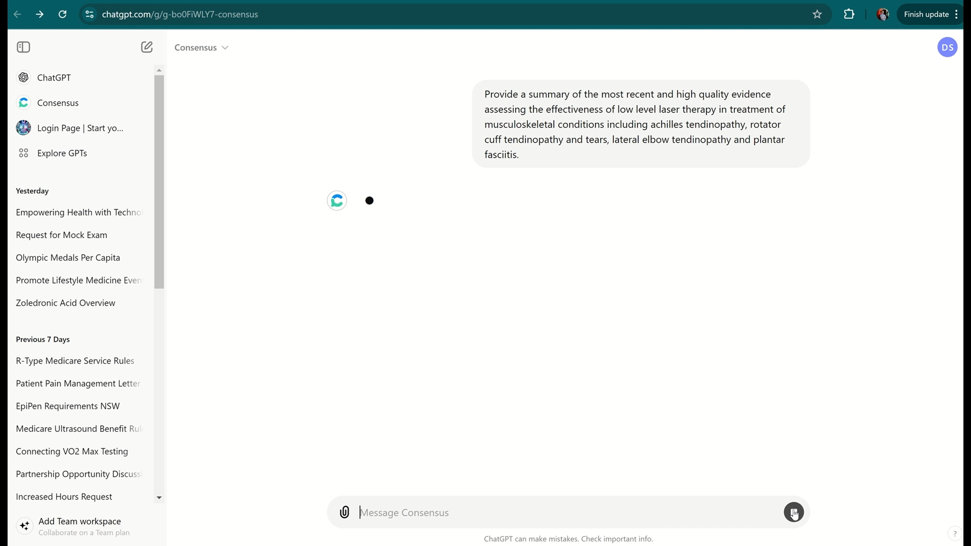
Harnessing AI for Better Decision-Making
Generative AI is revolutionizing healthcare, speeding up software development, and enabling smarter, data-driven decisions. Tools like ChatGPT are invaluable in creating policies, answering clinical questions, and providing the latest evidence summaries. For instance, I recently used AI to assess a potential $30,000 investment in laser therapy. By asking the right questions, I made an informed decision, highlighting how AI can help us make better choices in patient care

Advanced Testing and Assessments
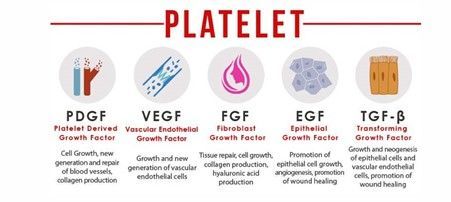
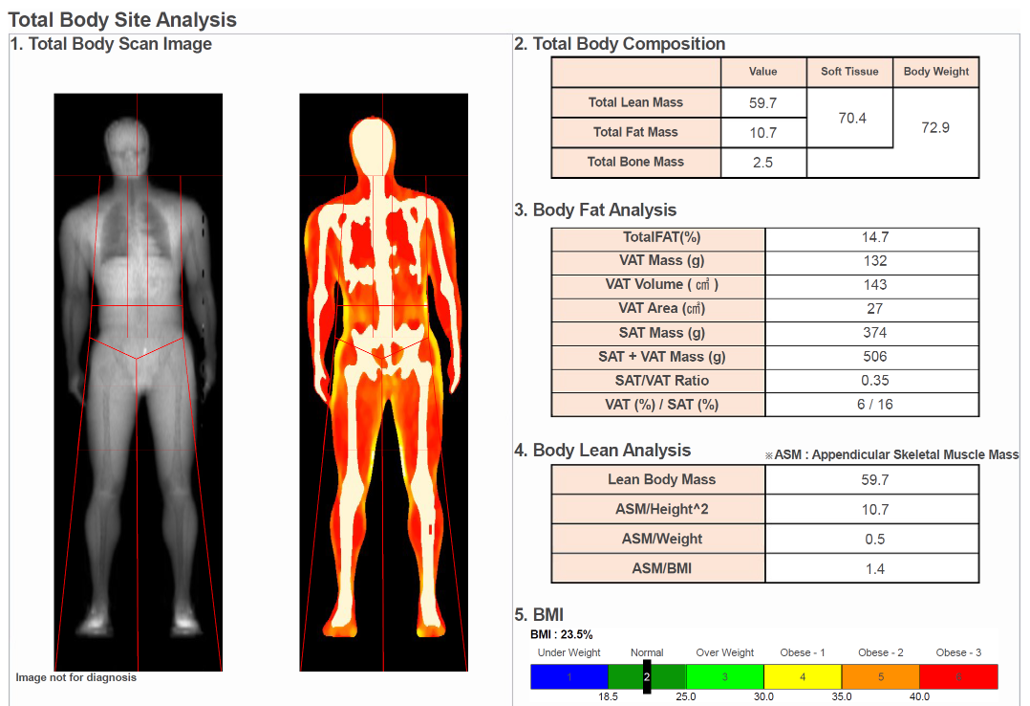
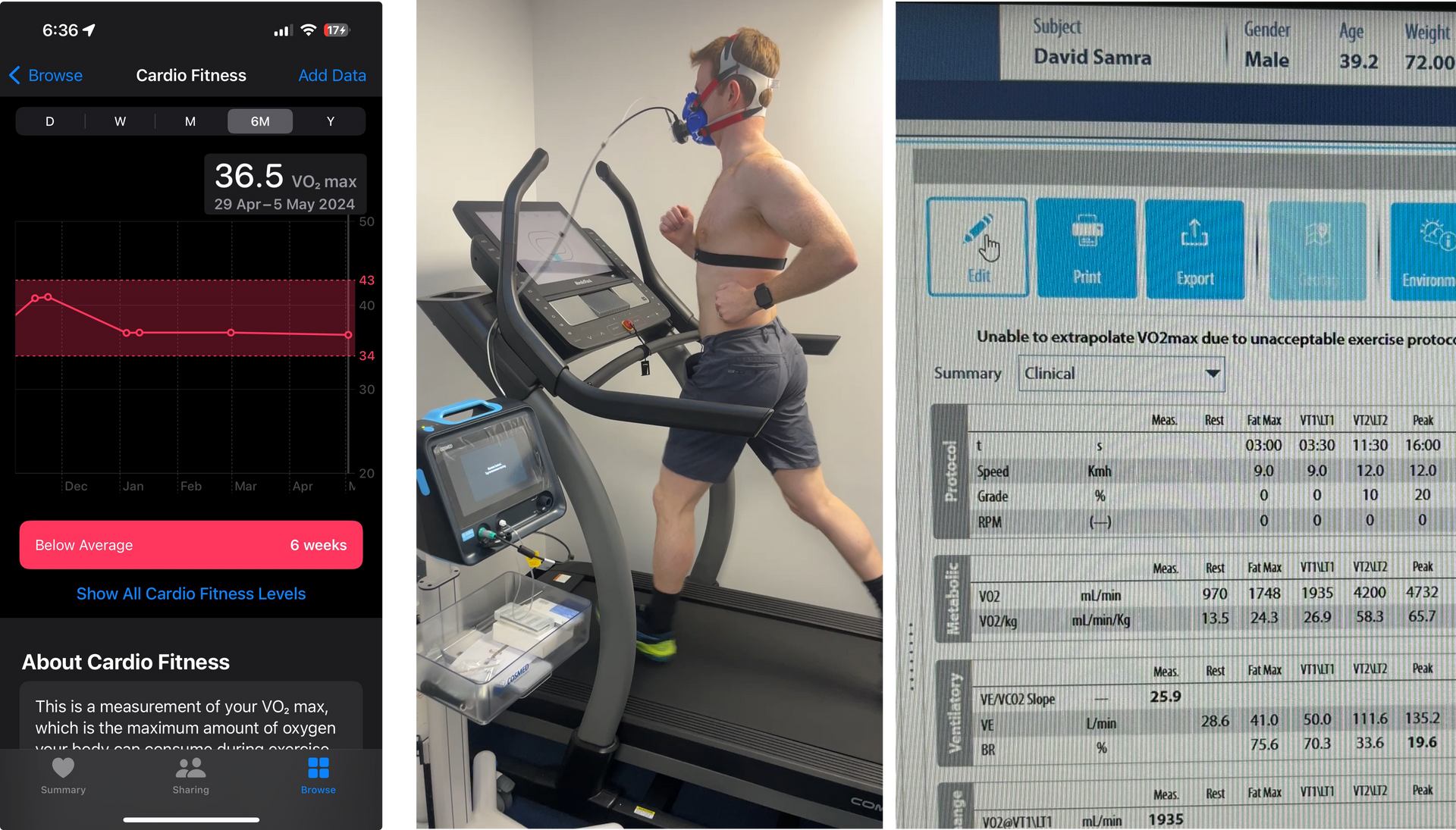
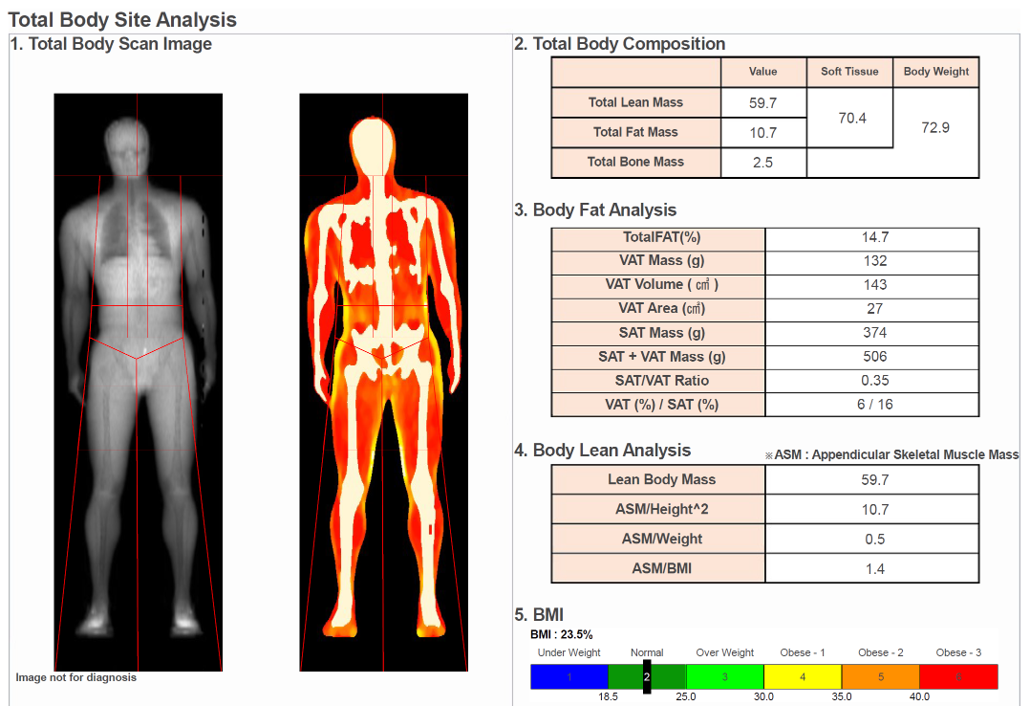
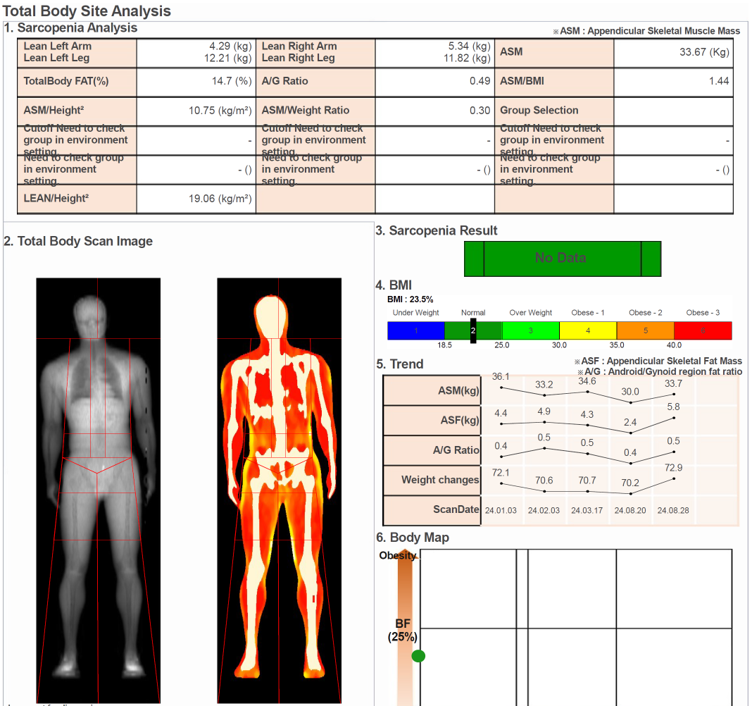
At Progressive Sports Medicine, we utilize advanced testing and assessments to provide personalized, data-driven care. Respiratory Exchange Ratio (RER) testing, VO2 Max assessments, and DEXA scans are just a few of the tools we use to tailor health and fitness strategies for our patients. These tests provide insights into metabolic function, cardiovascular fitness, and body composition, enabling us to develop targeted interventions for each patient.
At PSM, we do testing on ourselves too. You can see that my own VO2 max was grossly underestimated by Apple Watch, and the actual test came in at a much more respectable level. This technology ensures that we as clinicians, are leading by example and practicing what we preach.
These are my recent DEXA scan results indicating improving muscle mass and reducing visceral fat. I know that I need to do more work on my bone mass- that is my main area of deficiency and I wouldn't know this without this technology.
Our purpose built gym allows us to perform advanced strength testing and intervention. Strength measures are an important metric for rehabilitation, but also for overall healthspan and longevity.

The Hawthorne Effect: A Positive Force in Patient Care
The Hawthorne effect, often seen as a bias, can actually be harnessed to improve patient outcomes. When patients know they are being observed, they are more likely to adhere to their treatment plans. This increased engagement not only leads to better outcomes but also provides a clearer picture of the effectiveness of our interventions.
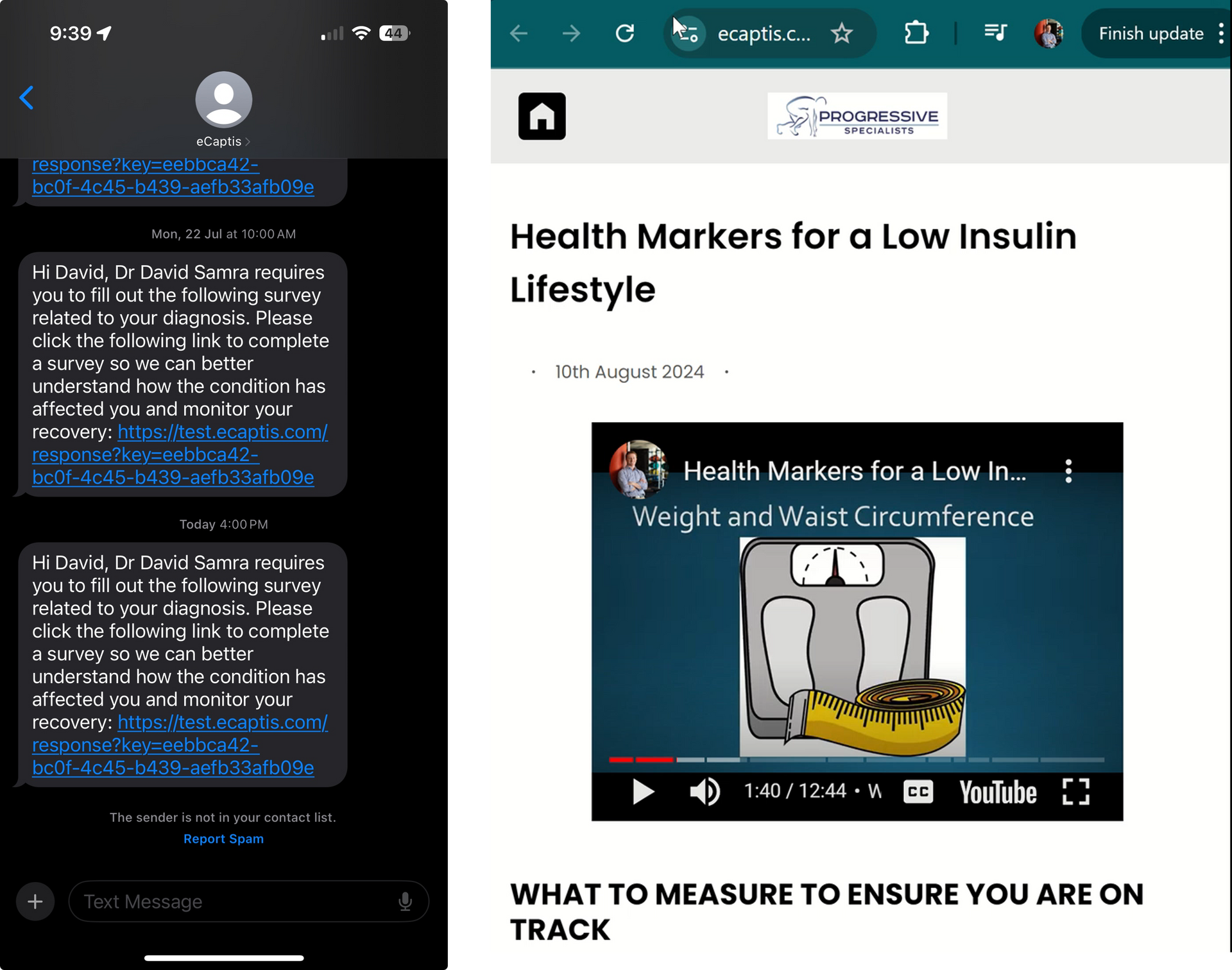
We are affiliated with Sydney University and the data and outcome measures we obtain from our patients not only helps us to help them, but it can contribute to peer reviewed research that assists our overall understanding of real-world clinical problems. After a long and tiresome search, we are glad to have partnered with eCaptis who are the best in class technology in Australia for measurement of outcome measures in clinical practice.
eCaptis allows us to seamlessly integrate patient outcome measures and results into our practice, and to create care pathways that provide educational content to patients along their journey of recovery.
Conclusion
As healthcare providers, our patients expect more from us than ever before. By integrating technology and embracing collaboration, we can enhance patient outcomes and streamline our practices. It's an exciting time to face the future fearlessly, using technology to centralize data and deliver the best care possible. At PSM, this is part of ensuring that we remain at the forefront of healthcare innovation