"What about Stem Cells doc?"
The Efficacy and Safety of Stem Cells in Treating Osteoarthritis
Can we replenish the worn cartilage in joints with Osteoarthritis?
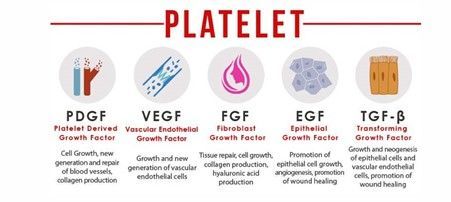
The current fascination with using mesenchymal stem cells (MSCs) for the treatment of osteoarthritis rests heavily on their potential to aid in regenerative medicine, particularly through mechanisms like angiogenesis—where these cells help in wound healing not by transforming into required cell types but by promoting new blood vessel formation. However, when it comes to actual, tangible evidence of these cells regenerating high-quality articular cartilage, the proof remains frustratingly elusive. Studies might show some symptomatic relief, but radiographs or MRI scans that confirm definitive cartilage regeneration are notably absent.
The Basic Science: What is a stem cell?
Stem cells are the foundation for every organ and tissue in the body and have unique regenerative abilities because they can proliferate (renew/divide) and "differentiate" (develop) into any cell type in the body to allow the specialised functions of those cells- from heart muscle cells to neurones in the brain. They are broadly categorized based on their potency, or the range of cell types they can become. Pluripotent cells can develop into almost any cell type in the body. Multipotent cells, including mesenchymal stem cells (MSCs) derived from bone marrow or adipose tissue, can differentiate into a more limited range of cells within a specific lineage.
Embryonic stem cells (ESCs), derived from early-stage embryos, are pluripotent and can differentiate into almost any cell type, making them highly valuable for research and potential therapies. Induced pluripotent stem cells (iPSCs) are adult cells that have been genetically reprogrammed to an embryonic stem cell-like state, also possessing the ability to develop into nearly any cell type. In therapeutic contexts, autologous stem cells are harvested from the patient’s own body, such as from fat or bone marrow, ensuring compatibility and reducing rejection risks. Allogeneic stem cells, such as those derived from umbilical cord blood, are sourced from donors, and are used in a variety of treatments, especially for blood and immune-related diseases.
A Brief History of Stem Cells
As is often the case in medicine, pre-clinical trials generated great enthusiasm and hope, but the translation to real world treatment has been disappointing. We have been able to use stem cells for osteoarthritis since the 2010's- in various forms. To understand where we are going, you need to know where we have come from with this technology, so here is a brief timeline.
In 1956, Dr Edward Donnall Thomas performed the first successful bone marrow (haematopoietic stem cell) transplant in a patient with inability to produce new blood cells from their bone marrow, due to blood cancer and it's treatment. This is now an established treatment, with evidence of effectiveness for certain cancers
In 1998, James Thomson isolated the first human embryonic stem cells. This made it possible to have new transplantation methods or various cell types for testing new treatments and drugs. Being embryonic, this raised significant ethical debate about cells that could form a human being sacrificed for research and medicine
In 2006, fibroblasts (collagen producing cells) were converted into the first pluripotent stem cells by Shinya Yamanaka's team in Kyoto, Japan. This technology offers a promising path for regenerative medicine by avoiding the ethical issues associated with the use of embryonic stem cells.
In 2013, I started my Specialist Medical training in Sports Medicine after 3 years of working in the hospital system and in Critical Care medicine. At around that time, stem cells were just being introduced into clinical practice, with biotechnology companies working closely with doctors as "early adopters", to deliver this innovative technology to patients in the office. Patients were able to access mesenchymal stem cells either derived from their abdominal fat (fat-derived), bone marrow and even via off-the-shelf donor stem cells, such as Progenza. Up until 2018 in Australia, there was minimal regulation of the procedures, as the processing of human tissue was not considered a drug requiring approval and had escaped the scrutiny of regulators. Since this time, stem cell treatments for Osteoarthritis have largely been quarantined within Registered Research Trials such as SCUlpTOR in hospital settings, to maximise trustworthiness of data that is gained about safety and effectiveness.
The practicality of stem cell treatments for osteoarthritis is debatable due to their high costs, the ambiguous nature of their effectiveness, and the risks associated with treatments, especially in unregulated environments often linked with medical tourism. The potential physical risks, while possibly minimal, are overshadowed by the severe financial implications of such expensive and unproven treatments. The mechanisms of action, while scientifically intriguing, offer little reassurance to those seeking more than anecdotal evidence of success.


Commercial Conflicts of Interest
The allure of these treatments is amplified by aggressive commercial interests and insufficient regulatory oversight, creating a precarious situation for patients drawn by the unverified promise of MSC therapies. Professional bodies like the Australasian College of Sport and Exercise Physicians are rightly cautious, advocating for the integration of MSC therapies into clinical practice only when backed by solid, reproducible evidence of their safety and effectiveness.
Australia’s Therapeutic Goods Administration (TGA) reinforces this cautious stance, noting that the only stem cell treatment proven safe and effective so far is hematopoietic stem cell transplantation for certain blood disorders and immune system conditions. The stark warning about the dangers of unproven stem cell treatments—ranging from infections to potentially severe allergic reactions—is a sobering reminder of the risk involved in pursuing such therapies, particularly in an unregulated, unfamiliar environment away from home. However, the theoretical risks of severe immune rejection or cancer formation (tumorigenesis), have not been substantiated in early clinical trials for joint injections and are probably negligible risks in reality.
The Hard Word on Stem Cells
While stem cell therapy holds a compelling allure due to its potential to revolutionize treatment paradigms, the actual benefits for osteoarthritis patients remain speculative at best, clouded by high costs, safety concerns, and a significant lack of conclusive evidence. The road to mainstream acceptance and application of MSC therapies in osteoarthritis treatment is fraught with scientific and ethical potholes that need careful navigation through rigorous clinical research and regulatory scrutiny.
I truly believe that Stem Cell therapy will revolutionise the way we treat Osteoarthritis and other injuries and degenerative conditions. However, until the methods of delivery can allow for actual cell differentiation and integration into the existing tissue, those who spend money on this treatment are either paying for a potent anti-inflammatory or an expensive placebo.
References and Links:
Clinical Trials Registry - Stem Cells in Osteoarthritis
TGA- Stem Cell Treatments and Regulation- A quick guide for Consumers
Park YB, Ha CW, Lee CH, Yoon YC, Park YG. Cartilage Regeneration in Osteoarthritic Patients by a Composite of Allogeneic Umbilical Cord Blood-Derived Mesenchymal Stem Cells and Hyaluronate Hydrogel: Results from a Clinical Trial for Safety and Proof-of-Concept with 7 Years of Extended Follow-Up. Stem Cells Transl Med. 2017 Feb 1;6(2):613–21.
Yubo M, Yanyan L, Li L, Tao S, Bo L, Lin C. Clinical efficacy and safety of mesenchymal stem cell transplantation for osteoarthritis treatment: A meta-analysis. PLoS ONE. 2017 Apr 27;12(4):e0175449.
Kuah D, Sivell S, Longworth T, James K, Guermazi A, Cicuttini F, et al. Safety, tolerability and efficacy of intra-articular Progenza in knee osteoarthritis: a randomized double-blind placebo-controlled single ascending dose study. J Transl Med. 2018 Mar 6;16(1):49.
Kingery MT, Schoof L, Strauss EJ, Bosco JA, Halbrecht J. Online Direct-to-Consumer Advertising of Stem Cell Therapy for Musculoskeletal Injury and Disease: Misinformation and Violation of Ethical and Legal Advertising Parameters. J Bone Joint Surg Am. 2020 Jan 2;102(1):2–9.
Lim HC, Park YB, Ha CW, Cole BJ, Lee BK, Jeong HJ, et al. Allogeneic Umbilical Cord Blood–Derived Mesenchymal Stem Cell Implantation Versus Microfracture for Large, Full-Thickness Cartilage Defects in Older Patients: A Multicenter Randomized Clinical Trial and Extended 5-Year Clinical Follow-up. Orthop J Sports Med. 2021 Jan 1;9(1):2325967120973052.
Wiggers TG, Winters M, Van Den Boom NA, Haisma HJ, Moen MH. Autologous stem cell therapy in knee osteoarthritis: a systematic review of randomised controlled trials. Br J Sports Med. 2021 Oct;55(20):1161–9.
Kim KI, Lee MC, Lee JH, Moon YW, Lee WS, Lee HJ, et al. Clinical Efficacy and Safety of the Intra-articular Injection of Autologous Adipose-Derived Mesenchymal Stem Cells for Knee Osteoarthritis: A Phase III, Randomized, Double-Blind, Placebo-Controlled Trial. Am J Sports Med. 2023 Jul;51(9):2243–53.
Kim KI, Lee WS, Kim JH, Bae JK, Jin W. Safety and efficacy of the intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritic knee: a 5-year follow-up study. Stem Cells Transl Med. 2022;11(6):586-596.
Sadri B, Hassanzadeh M, Bagherifard A, Mohammadi J, Alikhani M, Moeinabadi-Bidgoli K, et al. Cartilage regeneration and inflammation modulation in knee osteoarthritis following injection of allogeneic adipose-derived mesenchymal stromal cells: a phase II, triple-blinded, placebo controlled, randomized trial. Stem Cell Res Ther. 2023 Jun 14;14(1):162.
Karanes C, Nelson G, Chitphakdithai P, Agura E, Ballen KK, Bolan CD, et al. Twenty Years of Unrelated Donor Hematopoietic Cell Transplantation for Adult Recipients Facilitated by the National Marrow Donor Program. Biol Blood Marrow Transplant. 2008 Sep 1;14(9):8–15.