RMR Testing: The Key to Understanding Your Metabolism and Fuelling Smarter Fat Loss
RMR Testing Explained

If you’ve been training consistently, tracking your food, and still not seeing results — you’re not alone. I see it all the time. One of the most common missing links? Metabolism.
Your Resting Metabolic Rate (RMR) is the number of calories your body burns at complete rest — just to stay alive. That includes things like breathing, digesting food, circulating blood, and keeping your organs ticking. It actually makes up 60–75% of your daily energy expenditure — and if you don’t know this number, you're guessing.
At Progressive Sports Medicine, I use clinical-grade RMR testing to measure this in real time — no calculators, no assumptions, just real data from your breath.
Why Knowing Your RMR Actually Matters
Not everyone burns calories the same way. Two people with the same age, height, and weight could have completely different metabolic needs.
Online calculators? They often over- or underestimate by 200 to 600 calories. That’s a huge margin for error. If you’re under-eating by that much, it could stall fat loss, mess with your hormones, and eat into your muscle.
With an RMR test, we can accurately determine:
- How many calories your body needs at rest (RMR in kcal/day)
- Your Respiratory Exchange Ratio (RER) – showing whether you burn mostly fat or carbs at rest
- Your fat vs carbohydrate burning ratio (%)
- Energy output per litre of oxygen consumed (kcal/L O₂) – giving insight into your metabolic efficiency
- Crossover point – where your body shifts from fat-dominant to carb-dominant fuel use
- How your metabolic profile compares to normative data for your age and training status
This gives us a full picture — not just of how many calories you burn, but how your body prefers to use fuel.
What to Expect from Your RMR Test
It’s simple, calm, and non-invasive. Here’s how it works:
- You come in fasted (no food, caffeine, or exercise beforehand). 8+ hours
- You’ll lie down, breathe while sitting under a canopy for 15–20 minutes.
- The system measures your oxygen and carbon dioxide exchange.
- I interpret the results and walk you through what they mean.
Real Story: Lisa’s Fat Loss Plateau
Lisa came in frustrated. She was eating 1,200 calories a day, training five times a week, but nothing was changing — and she felt flat.
Her RMR test showed:
- RMR: 1,450 kcal/day
- RER: 0.92 (very carb-reliant, low fat-burning)
She was under-fuelling and stuck in a high-stress metabolic state. We bumped her calories to 1,700, restructured her macros, and focused on strength training. Six weeks later? She dropped 2.5kg of fat and felt energised for the first time in months.
Who Should Do RMR Testing?
- Anyone trying to lose weight or struggling with a plateau
- Athletes looking to fine-tune fuelling and recovery
- Individuals recovering from injury or surgery
- Women over 35, especially those dealing with hormonal shifts
- Anyone who’s been dieting for years or doing HIIT with no results
- Clients experiencing burnout, low energy, or muscle loss despite training hard
What You’ll Walk Away With
After your RMR session at
Progressive Sports Medicine, you'll get: Your true metabolic rate in calories/day
Your RER score and fat vs carb burning profile
A breakdown of metabolic efficiency and energy use
A full digital report explained by me, not just handed to you
Clear, customised strategies to apply straight away
It’s Not Just About Eating Less — It’s About Eating Smart
Understanding your metabolism changes everything. Whether you're trying to lose fat, protect muscle, or optimise performance, RMR testing gives you a tailored blueprint to work from.
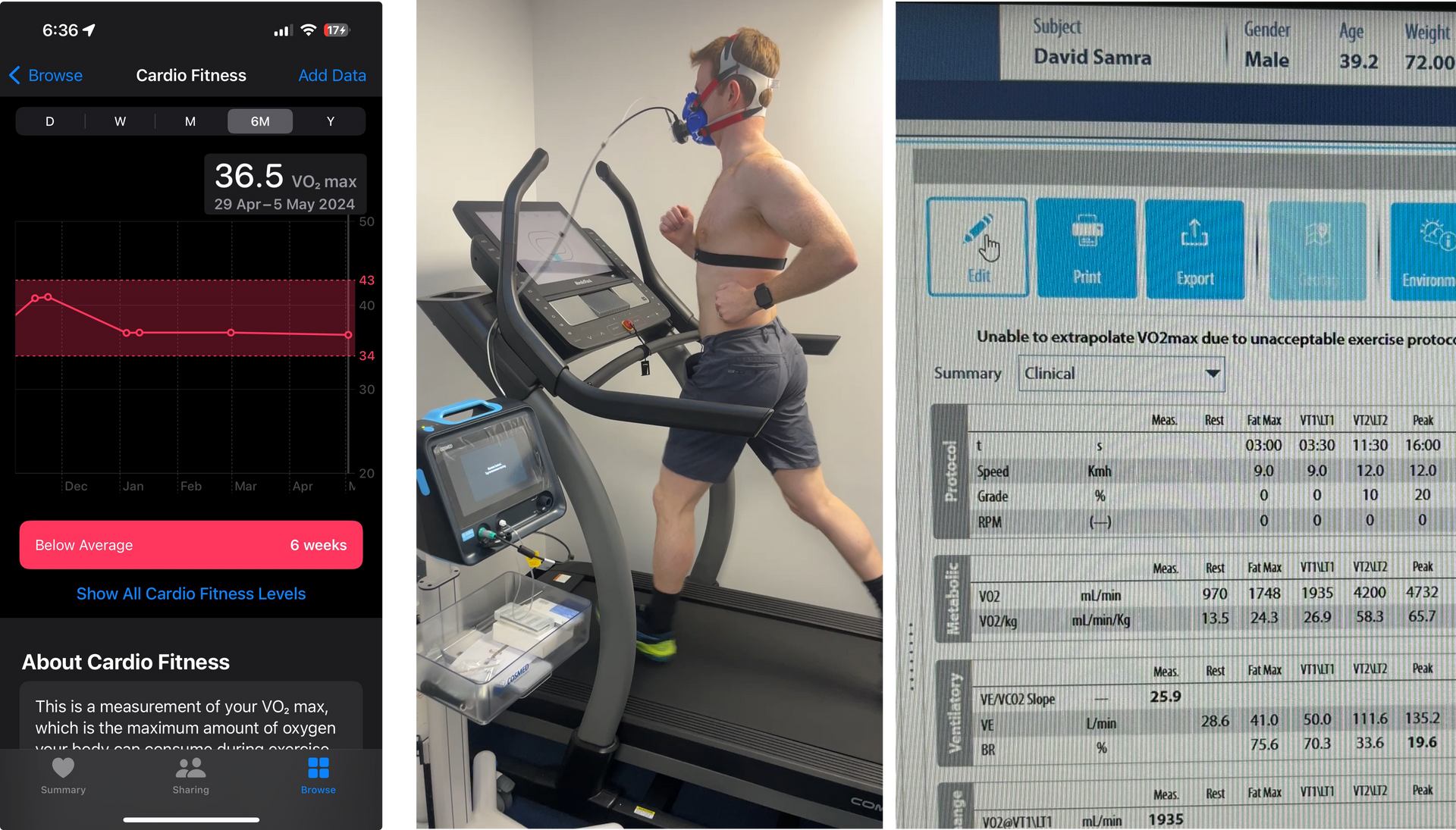
You will receive gold-standard metabolic testing in 20 minutes and expert interpretation by a qualified Exercise Physiologist (yours truly).
Train smarter. Fuel better. Progress faster.